Periodontitis – from inflammation of the gums to inflammation of the tooth socket
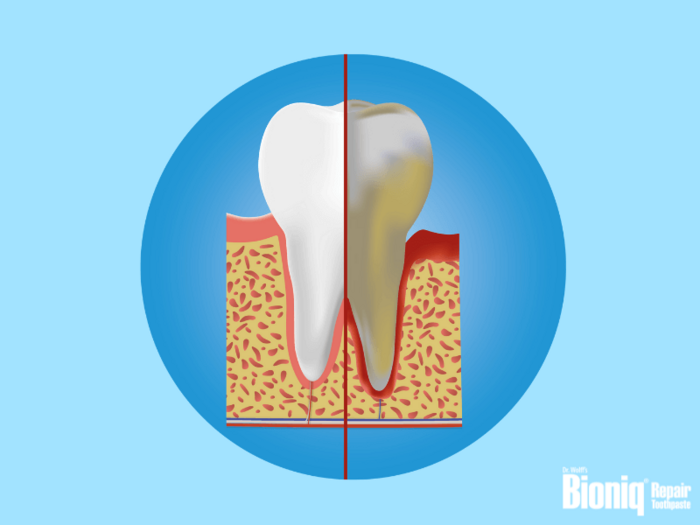
In layman's terms, periodontitis is also commonly known as gum disease. It is a bacterial disease of the gums and the periodontium and refers to inflammation of the tooth socket. The tooth socket is made up of the gums and cementum, and connects the tooth to the jaw. In periodontitis, the inflammation damages the periodontal apparatus (the tissues supporting a tooth) and can, at worst, lead to the loss of individual teeth.
Periodontitis is often preceded by gingivitis. This inflammation initially only affects the gums. It is an extremely insidious disease, as in the early stages, patients notice only a few or even no symptoms. This means that gingivitis often goes unnoticed: bacteria can proliferate in hard-to-reach areas; inflammation becomes advanced and turns into periodontitis.
In this article, you will find out how to recognise periodontitis, how to treat it and how to prevent it.
Periodontitis as a result of gingivitis
![[Translate to en_SG:] Periodontitis as a result of gingivitis [Translate to en_SG:] Periodontitis as a result of gingivitis](/fileadmin/user_upload/bioniq-repair-zahnpflege.com/images/content/zahngesundheit/zahnfleischentzuendungen/bioniq-repair-teaser-zahnfleischentzuendung_.jpg)
Inflammation of the gums – known as gingivitis – is not rare and affects almost all adults at least once in their lives. It occurs when oral hygiene is inadequate. Bacteria build up on the gum line, where they can trigger an inflammatory reaction. The first signs can be bleeding of the gums and bad breath.
Gingivitis is usually harmless and resolves itself quickly with improved oral care. However, if it persists, periodontitis can develop insidiously as a result.
In periodontitis, the bacteria are transmitted from the gums to the tooth socket, where periodontal pockets are formed. The tooth then loosens from the gums and a gap arises. These grooves are ideal spots for bacteria, as they can proliferate here almost undisturbed. A toothbrush and dental floss cannot reach the periodontal pockets.
The remains of food which bacteria feed on also remain in the pockets, providing them with optimal living conditions. The bacteria then penetrate even further into the periodontium. Finally, the bacteria are able to reach, attack and damage the jawbone and the cementum.
Furthermore, the body also responds to the infection by sending osteoclasts (bone-destroying cells) to defend against the bacteria. The consequences: the function of the periodontium is then impaired and tooth loss may occur.
Causes of and risk factors for periodontitis
The most common cause of periodontitis is inadequate oral hygiene, resulting in a bacterial load in the mouth. Generally, periodontitis precedes gingivitis. Therefore, you should avoid the following risk factors:
- Correct oral hygiene: Clean your teeth thoroughly at least twice a day to remove plaque and food residue – this is how you can prevent cavities.
- Avoid infection: It is possible to catch periodontitis. Therefore, you should not share your toothbrush or use the same cutlery as your partner or child.
- Tartar: If necessary, ask your dentist to remove the tartar from your teeth. Tartar occurs when plaque "calcifies". As a result, grooves are formed which present the perfect environment for the adhesion of bacteria.
- Smoking: 70% of people with periodontitis are regular smokers. The reason: nicotine impairs circulation, and as a result, the body is less able to fight gum infections.
There are also other risk factors which are harder to control:
- Predisposition: Periodontitis often occurs repeatedly within a family.
- Hormonal fluctuations: During pregnancy and puberty, the risk of bacterial infections in the oral cavity increases.
- Preexisting conditions: Many predispositions can also increase the risk of periodontitis. Diabetes mellitus impacts the circulation, which has a negative effect on immunity. In HIV, the immune system is weakened and is less able to respond effectively to infections.
Periodontitis – treatment by a dentist
Before treatment comes the diagnosis. First, your dentist can use the periodontal screening index (PSI) to determine the progression (stage) of the periodontitis. Jaw X-rays are also taken to detect any possible bone loss. Then the appropriate treatment steps are decided on the basis of these results.
The treatment of infection of a dental socket comprises various escalation stages according to the degree of progression, and the dentist will decide which is appropriate. A basic treatment is usually performed at the start of therapy. If this is not sufficient, further steps can be taken, such as minor surgery.
The primary objectives of the treatment of periodontitis are to limit the proliferation of bacteria, therefore also halting gingivitis and inflammation of the periodontium, at the same time preserving the tissues.
Basic treatment of periodontitis
First the teeth need to be cleaned and plaque/tartar removed. To do so, the dentist will initially perform a basic treatment. Local anaesthesia is necessary for the procedure known as closed curettage . Then the dentist will remove the tartar around the necks of the teeth and the gums, either manually or using medical instruments (e.g. ultrasonic devices). In some circumstances, a laser can also be utilised to remove the affected tissue, which also has an antibacterial effect. Antibiotics may also be necessary. This basic treatment is often enough to halt the progress of the infection and to reduce the symptoms.
Surgical treatment of periodontitis
If periodontitis is extremely aggressive or advanced, or it has not been possible to completely halt the inflammation using the closed periodontitis treatment, open treatment in the form of surgery will be necessary. First, the dentist opens any particularly deep gingival pockets slightly, to combat the bacteria directly and to detect and remove any diseased tissue. The gums can then replaced to fit against the tooth, to limit the adhesion of bacteria in the future.
If the periodontium is already affected and the attachment of the teeth is threatened, a tissue transplant may be needed. For this purpose, one option is to excise the required tissue from the patient's palate for transplantation. So-called transposition flaps can also be used. For this purpose, healthy gum tissue is excised and transposed onto the infected area. The two methods are often combined to achieve a cosmetically flawless finish.
If the bone is also affected, it can be replaced using the patient's own bone tissue or a bone substitute.
Preventing periodontitis
So that treatment of periodontitis or surgery is never needed in the first place, we recommend preventive measures. The following tips will help you to prevent inflammation of the tooth socket:
- Practise regular and thorough oral care by brushing your teeth in the morning and evening. Also use dental floss or interdental brushes to clean the spaces between your teeth. The use of mouthwash to minimise the bacterial load in the oral cavity is also recommended.
- Try to eat a healthy diet and avoid the excessive consumption of sugary drinks throughout the day. Ideally, sweet things should be eaten immediately after a main meal so that the bacteria do not have a continuous new food supply.
- Attend the six-monthly check-up appointment at your dentist, so that periodontitis can be detected at an early stage.
- Regularly have your teeth professionally cleaned (scale and polish) at your dental surgery. During treatment, the teeth are not only cleaned: potential risk factors are also detected.
- Try to limit nicotine consumption or ideally, give up smoking. The risk of periodontitis is significantly elevated in smokers.
Secondary diseases in periodontitis
Left untreated, periodontitis can also have other dangerous consequences alongside possible tooth loss: studies have shown a correlation between periodontitis and cardiovascular diseases, as the bacteria can penetrate the coronary vessels through the bloodstream. The respiratory system can also be affected by pathogens, which can sometimes cause pneumonia.
You may also be interested in:

Inflammation of the gums (gingivitis)
If your gums are reddened, swollen or even bleeding, these may be signs of gingivitis. In this article you will learn how to detect inflamed gums, how good oral hygiene promotes healing and when gingivitis means a visit to the dentist.

Sensitive teeth
Individuals suffering from sensitive teeth know the sudden, flash-like pain which will follow after savouring cold, hot, sour or sweet foods. Here, you will find the most frequent causes for the so-called dentin hypersensitivity and what you can do about it!

![[Translate to en_SG:] Periodontitis – treatment by a dentist [Translate to en_SG:] Periodontitis – treatment by a dentist](/fileadmin/user_upload/bioniq-repair-zahnpflege.com/images/content/zahngesundheit/parodontitis/bioniq-repair-teaser-parodontitis-behandlung-zahnarzt.jpg)
![[Translate to en_SG:] Preventing periodontitis [Translate to en_SG:] Preventing periodontitis](/fileadmin/user_upload/bioniq-repair-zahnpflege.com/images/content/zahngesundheit/parodontitis/bioniq-repair-teaser-parodontitis-praevention.jpg)
